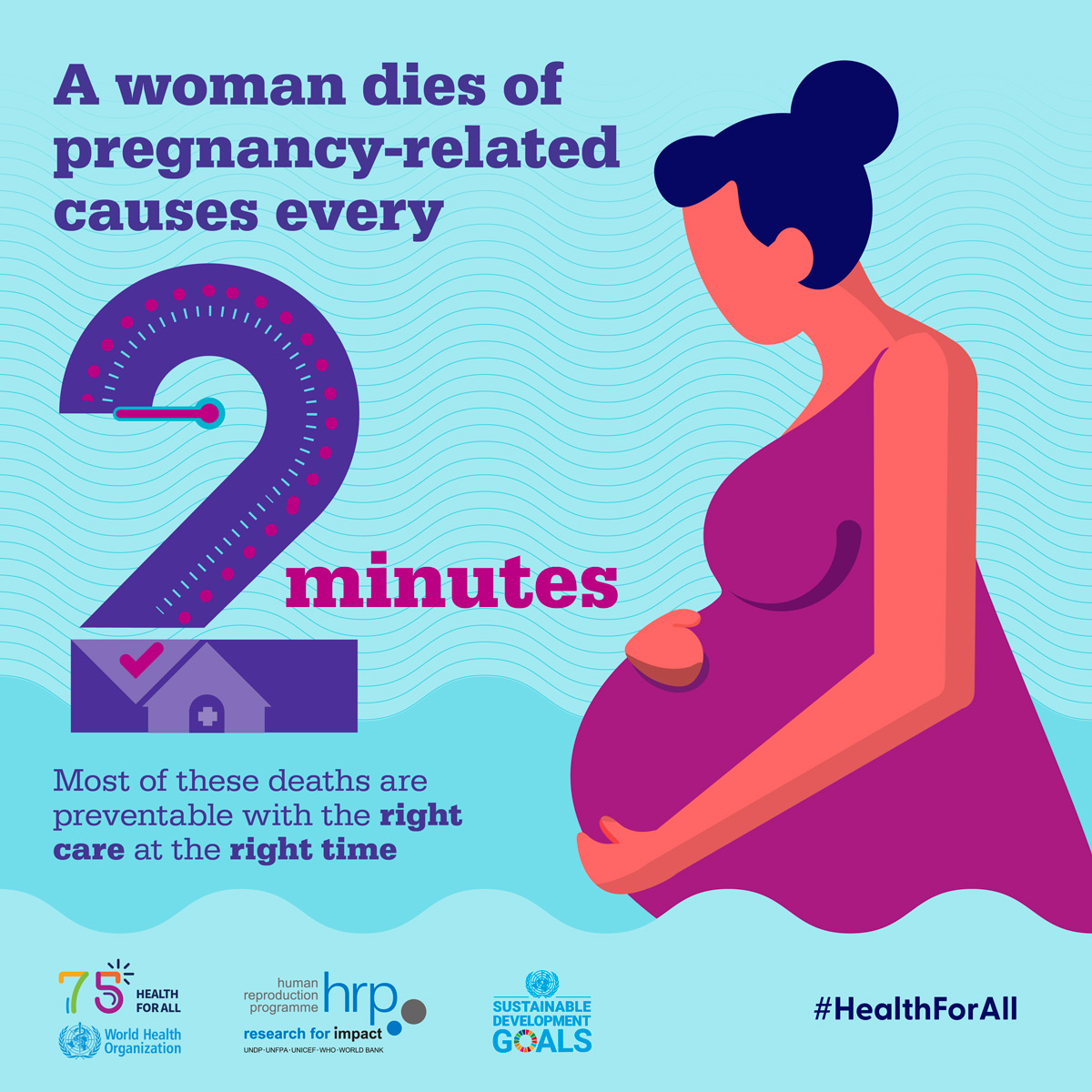
Maternal mortality remains a critical issue in the United States, with the nation recording the highest rates of pregnancy-related deaths among its high-income counterparts. Alarmingly, more than 80 percent of these fatalities are deemed preventable, pointing to systemic flaws within the maternal health care system. Recent studies indicate that between 2018 and 2022, the maternal mortality rate has only risen, exacerbating existing racial disparities in maternal care that disproportionately affect women of color. The increase in deaths is a wake-up call for improved prenatal care and robust postpartum care to ensure a safer journey for mothers. Addressing preventable deaths in pregnancy is essential not only for enhancing maternal health outcomes but also for fostering equity in health care access across diverse communities.
The transition of focus towards maternal health encompasses various terminologies such as pregnancy-related fatalities and childbirth mortality. In the broader context of women’s health, understanding the complexities of postpartum care and its implications can lead to significant reductions in preventable deaths during pregnancy. Often, the discussion veers towards the alarming racial disparities in maternal care, which highlight the urgent need for equitable health strategies. Innovative approaches are crucial to address these challenges and enhance the care continuum from conception to beyond childbirth. Recognizing the multifaceted nature of maternal health is a vital step toward improving outcomes for all mothers.
Understanding the Rise in Maternal Mortality
In recent years, the United States has witnessed a troubling trend: an increase in maternal mortality rates, which stands in stark contrast to the improvements seen in many other high-income countries. This rise is alarming, especially considering that over 80% of these pregnancy-related deaths are deemed preventable. Factors contributing to this situation include a fragmented healthcare system, inequitable access to care, and historical biases against racial and ethnic minorities. Addressing these issues requires a concerted effort to rethink our maternal healthcare policies and ensure that all women receive adequate care throughout their pregnancies.
Moreover, the surge in maternal deaths has unveiled significant disparities linked to race and geography, with certain demographics disproportionately affected. For example, American Indian and Alaska Native women face the highest maternal mortality rates compared to white women. This indicates that the systems in place not only fail to provide equal care but may also perpetuate existing health inequalities. To tackle these challenges, stakeholders must prioritize comprehensive reforms targeted at improving maternal health equity across all population groups.
Given the systemic issues, a unified national strategy is essential to address the factors driving the rising rates of maternal mortality. Experts suggest that focusing on preventative measures and enhancing both prenatal and postpartum care could significantly alleviate the burden of pregnancy-related deaths. By investing in a healthcare framework that prioritizes the needs of diverse communities, we can shift towards a system that truly safeguards maternal health.
Furthermore, pregnant individuals must have access to a broader spectrum of support that accounts for chronic conditions that could arise during pregnancy, including cardiovascular diseases. The evidence gathered from various studies indicates that the healthcare system needs to adapt to the changing demographics and health profiles of pregnant individuals, thus averting avoidable deaths.
Racial Disparities in Maternal Health Outcomes
The racial disparities prevalent in maternal health outcomes have been a persistent issue in the United States. Recent studies have established a clear link between race and maternal mortality, with non-Hispanic Black women and American Indian/Alaska Native women experiencing significantly higher rates of pregnancy-related deaths compared to their white counterparts. This disparity highlights the urgent need for targeted interventions that address the root causes of these inequities, including social determinants of health and historical biases entrenched in healthcare practices. Addressing these disparities is not only a matter of public health but also of social justice.
To confront these racial disparities effectively, healthcare systems must implement culturally competent care practices and provide comprehensive training to healthcare providers. Programs that focus on improving communication, understanding cultural differences, and addressing implicit biases can strengthen the doctor-patient relationship and ensure that care is more equitable. Enhanced community engagement and outreach can also play a crucial role in improving access to quality prenatal and postpartum care for underserved populations.
Furthermore, policies aimed at increasing funding for maternal health programs in high-risk communities are essential. These programs should encompass a multidisciplinary approach that integrates mental health support, chronic disease management, and continuous health education. By creating an inclusive environment that prioritizes the unique needs of different racial groups, we can work toward significantly reducing the maternal mortality rates affecting these populations.
Ultimately, it is imperative to foster new policies and practices that focus on eliminating health disparities, ensuring that all mothers, regardless of their racial background, have equitable access to safe and effective maternal care.
The Importance of Extended Postpartum Care
Postpartum care is an often overlooked yet critical component of maternal health that can significantly impact mortality rates. Recent research indicates that nearly a third of pregnancy-related deaths in the United States occur during the postpartum period, highlighting the necessity for extended care that goes beyond the conventional six-week check-up. This period of recovery is crucial for detecting and managing potential complications that may arise after childbirth, such as maternal depression or chronic health issues, like hypertension or cardiac conditions.
Implementing policies advocating for extended postpartum care could lead to a decrease in preventable maternal deaths. This shift involves recognizing the postpartum phase as an integral part of maternal health, where continuous support and monitoring can help identify issues before they escalate into severe complications. By promoting holistic care models that emphasize mental and physical health during the entire first year after childbirth, we can significantly improve outcomes for mothers.
Moreover, providers need to devise individualized postpartum care plans that address the unique needs of each mother, including risk factors based on their personal and family health histories. Ensuring that follow-up visits are adequately spaced and that mothers are educated about what symptoms to monitor can lead to prompt intervention when necessary.
Through this comprehensive approach, we can redefine postpartum care as a continuum rather than a discrete event, ultimately fostering a supportive environment for new mothers that prioritizes their health and well-being.
Preventing Maternal Deaths Through Comprehensive Care
Preventing maternal deaths requires a collaborative approach that focuses on comprehensive care throughout the pregnancy and beyond. The alarming statistic that over 80% of pregnancy-related deaths are preventable highlights the urgent need for systematic changes within the healthcare framework. Effective prenatal care, which includes routine screenings, education on risk factors, and emotional support, lays the groundwork for healthier pregnancies and more favorable outcomes.
In addition to prenatal care, enhancing postpartum follow-up services plays a vital role in preventing complications that can lead to maternal mortality. The post-pregnancy phase is crucial for monitoring women’s health, addressing mental health needs, and managing chronic conditions that may worsen after childbirth. By empowering healthcare providers to offer thorough postpartum evaluations and support, we create an environment where mothers can thrive, not just survive.
Moreover, community-based interventions tailored to meet the specific needs of diverse populations can effectively mitigate the risks associated with pregnancy and childbirth. Programs that expand access to healthcare services for at-risk communities, particularly in maternity care deserts, are essential for closing the health equity gap and improving maternal health outcomes.
Investing in education and outreach initiatives can further enhance awareness of available resources for expecting and new mothers. By working collaboratively, healthcare systems can build a structure conducive to preventing pregnancy-related deaths and enhancing overall maternal health.
Challenges Facing the U.S. Maternal Health System
Despite advancements in medical knowledge and technology, the U.S. maternal health system faces numerous challenges that hinder progress in reducing maternal mortality rates. Key issues include disparities in healthcare access, quality of care, and the integration of services designed to support pregnant individuals. A patchwork healthcare system often leads to significant gaps in care, where many mothers do not receive appropriate evaluation or treatment for chronic conditions leading to pregnancy complications.
One significant challenge is addressing the varying maternal health outcomes across states and demographics. Research consistently shows that states like California have made strides in lowering maternal mortality rates, while others lag significantly behind. This inconsistency raises questions about healthcare policies, funding allocations, and the overall commitment to improving maternal care across the nation.
Building a cohesive system that ensures all mothers have equal access to quality healthcare is critical for addressing these challenges. A focus on expanding insurance coverage, improving educational resources, and promoting collaboration between community organizations and healthcare providers can enhance maternal care delivery.
Additionally, advocating for policies that prioritize maternal health funding will ensure that adequate resources are allocated to combat ongoing challenges, create sustainable programs, and ultimately save lives.
The Role of Research in Maternal Health Improvement
Research plays an essential role in understanding the dynamics of maternal health and effectively shaping policies for improvement. Recent studies provide valuable insights into the causes and risk factors associated with maternal mortality, helping to identify trends and disparities that necessitate targeted interventions. By evaluating data such as the rise in cardiovascular-related deaths during pregnancy, researchers can inform healthcare providers, policymakers, and communities about critical areas that require immediate attention.
Moreover, with the implementation of the pregnancy checkbox on death certificates, comprehensive and consistent tracking of maternal deaths has become possible. This advancement enables researchers to gather crucial data that reveal patterns and outcomes across different demographics and regions—information that is paramount in developing effective strategies for reducing preventable deaths in pregnancy. All stakeholders must recognize the importance of investing in maternal health research and utilize findings to implement evidence-based practices.
Future studies focusing on the long-term health impacts of maternity care inequalities, as well as the effectiveness of proposed interventions, will create a robust body of evidence driving systemic changes within the healthcare sector. By harnessing research to inform practice and policy, we can propel maternal health initiatives that address not only current disparities but also future challenges.
Thus, continued support for maternal health research will foster informed decision-making and ultimately enhance the well-being of mothers and infants across the nation.
Strategies for Enhancing Maternal Health Access
Enhancing maternal health access requires a multifaceted strategy that addresses barriers preventing women from receiving adequate care during and after pregnancy. Innovative approaches are necessary to create pathways for equitably serving diverse populations across varying socio-economic backgrounds. This can include expanding telehealth services, which have proven effective in reaching expectant women, especially in underserved areas where maternity care resources are limited.
Additionally, strengthening community outreach programs can empower women to take charge of their maternal health. Educational initiatives aimed at informing women about available resources, including prenatal classes, health screenings, and support services, can bridge gaps in knowledge and resources. Training community health workers to assist expectant mothers in navigating the healthcare system can significantly diminish access barriers.
Furthermore, health policies should be directed at improving transportation options for pregnant individuals who may encounter difficulties reaching healthcare facilities. Comprehensive initiatives that foster collaboration between public health agencies, healthcare providers, and community organizations are essential in creating supportive frameworks for mothers before, during, and after childbirth.
Ultimately, by implementing strategies that prioritize access and education, we can create a system where maternal health is accessible to all women, significantly reducing the preventable mortality associated with pregnancy.
Community Engagement in Maternal Health Initiatives
Effective community engagement is crucial for advancing maternal health initiatives, as grassroots involvement fosters trust and responsiveness within populations that may feel disconnected from traditional healthcare systems. To improve maternal health outcomes, communities must be actively involved in designing and implementing policies that reflect their specific needs and resources. Active engagement can lead to more relevant and culturally sensitive healthcare solutions.
Community-based organizations can play a pivotal role in raising awareness and providing education about maternal health issues, particularly in areas with high maternal mortality rates. By organizing workshops, informational sessions, and support groups, these organizations can empower women to advocate for their rights and access the healthcare they need. Involving local leaders and stakeholders in maternal health initiatives also ensures that efforts are sustainable and grounded in community realities.
Moreover, collaboration between community organizations and healthcare providers can foster partnerships that enhance maternal care delivery systems. These partnerships can help identify gaps in services, drive targeted interventions, and leverage resources to support holistic maternal health programs catering to local needs.
By prioritizing community engagement in maternal health initiatives, we can cultivate a more inclusive and effective healthcare environment that empowers mothers to access the care they deserve.
Investing in Maternal Health for Future Generations
To combat the increasing rates of maternal mortality, long-term investment in maternal health is paramount. This investment should not only encompass immediate healthcare services but also address the broader ecological factors influencing maternal health outcomes. Ensuring sufficient funding and resources are allocated for maternal health initiatives is critical for developing programs that can effectively reduce preventable deaths during pregnancy and the postpartum period.
Additionally, prioritizing maternal health in public health agendas can enhance infrastructure, leading to systemic changes aimed at improving care for all mothers. Advocacy for maternal health funding must be a collective effort, engaging stakeholders from healthcare, government, and community sectors who share the common goal of improving health outcomes.
Investing in maternal health education programs can also equip healthcare providers with the tools and knowledge required to deliver high-quality care. This includes training on recognizing indicators of potential complications and addressing societal factors that affect women’s health.
By cultivating a culture of investment and prioritizing maternal health, we can lay the foundation for healthier pregnancies and births, which will benefit generations to come.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S.?
Maternal mortality in the U.S. is largely attributed to chronic health conditions, particularly cardiovascular diseases, which contribute to over 20% of pregnancy-related deaths. Other significant causes include hemorrhage and postpartum complications. Factors such as inadequate healthcare access and racial disparities in maternal care further exacerbate these risks.
How does maternal mortality in the U.S. compare to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, with over 80% of pregnancy-related deaths being preventable. This stark contrast is due to a patchwork healthcare system, inequities in access to maternal health services, and systemic biases affecting various racial and ethnic groups.
What role do racial disparities play in maternal mortality rates?
Racial disparities significantly impact maternal mortality rates, with American Indian and Alaska Native women facing the highest risks, followed by non-Hispanic Black women. These disparities highlight the urgent need for systemic reforms in maternal healthcare that address the inequities in access and treatment across racial lines.
What can be done to reduce preventable deaths in pregnancy?
To reduce preventable deaths in pregnancy, investment in comprehensive prenatal and postpartum care is essential. Policies must target healthcare access improvements and address the root causes of racial disparities in maternal health. Additionally, education and awareness campaigns can help expectant mothers recognize warning signs and seek timely care.
Why is postpartum care critical in addressing maternal mortality?
Postpartum care is crucial because nearly a third of maternal deaths occur after the initial 42 days following childbirth. Ensuring continuous care beyond the traditional six-week postpartum checkup is vital to monitor health conditions that may arise, thereby preventing late maternal deaths and improving overall maternal health outcomes.
How have maternal mortality rates changed during the COVID-19 pandemic?
During the COVID-19 pandemic, maternal mortality rates saw a sharp increase, particularly in 2021. This trend emphasizes the need for enhanced prenatal and postpartum care systems to mitigate the additional risks posed by the pandemic and ensure the safety of pregnant individuals.
What is the importance of tracking maternal mortality data?
Tracking maternal mortality data is crucial for identifying trends, understanding the underlying causes, and implementing effective interventions. The U.S. only began consistently tracking these deaths in 2018, which allows for more comprehensive data analysis to inform public health policies and improve maternal health outcomes.
What measures are suggested to improve maternal health outcomes?
Improving maternal health outcomes requires a multifaceted approach that includes increasing access to quality healthcare, addressing socioeconomic disparities, enhancing public health infrastructure, and advocating for equitable maternity care policies that encompass a full continuum of care from pregnancy through postpartum.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality Rates | The U.S. has the highest maternal mortality rate among high-income countries, continuing to rise from 2018 to 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable. |
| Disparities by Race | Significant racial disparities exist, with American Indian and Alaska Native women facing the highest rates of mortality. |
| Leading Causes | Cardiovascular disease has become the leading cause of pregnancy-related deaths, comprising over 20% of all cases. |
| Late Maternal Deaths | Nearly one-third of maternal deaths occur between 42 days and 1 year after pregnancy. |
| Healthcare System Challenges | The U.S. healthcare system’s structure is fragmented, leading to inequalities in care during and postpartum. |
Summary
Maternal mortality continues to be a critical issue in the United States, with rising rates highlighting significant disparities in healthcare access and outcomes. Understanding the preventable nature of most pregnancy-related deaths underscores the urgent need for systemic improvements in prenatal and postpartum care. Addressing these challenges could drastically reduce the mortality rates, benefitting women across all demographics and advocating for equity in maternal health.