Alzheimer’s research is pivotal in the quest to understand and combat one of the most challenging neurodegenerative diseases facing our aging population today. At the forefront of this effort is neuroscientist Beth Stevens, whose groundbreaking work at Boston Children’s Hospital sheds light on the role of microglial cells—the brain’s immune defenders. These cells are essential for maintaining brain health, yet their malfunction can contribute to the progression of Alzheimer’s and similar disorders. Stevens’ investigations have not only unveiled the complexities surrounding microglial behavior but also paved the way for innovative Alzheimer’s treatment strategies and the identification of biomarkers that promise earlier detection of these debilitating conditions. As the stakes rise with the increasing prevalence of Alzheimer’s, understanding these cellular mechanisms becomes crucial for developing effective new therapies that could transform lives.
The exploration of dementia-related disorders, particularly Alzheimer’s disease, has gained significant attention within scientific communities and healthcare facilities. Researchers have begun to unveil the mysteries surrounding microglial activity, which plays a crucial role in maintaining neuronal health and function. Associate professor Beth Stevens, based at Boston Children’s Hospital, is leading groundbreaking initiatives to unravel the intricate relationships between immune responses in the brain and the emergence of neurodegenerative diseases. The transformative insights derived from such studies are not only enlightening our understanding of Alzheimer’s but also guiding the future of effective treatments. As we delve deeper into this critical area of medical research, the potential for advancing Alzheimer’s therapy and improving patient outcomes becomes increasingly tangible.
Understanding Microglial Cells and Their Role in Alzheimer’s Disease
Microglial cells are essential components of the central nervous system (CNS) that act as the brain’s immune cells, continuously monitoring the environment for signs of damage or disease. In the context of Alzheimer’s disease, these cells take on a dual role; while they are responsible for clearing away dead neurons and other debris, they can also contribute to neurodegeneration when their functioning becomes flawed. Aberrant microglial activity has been implicated in various neurodegenerative diseases, where excessive pruning of synapses can lead to cognitive decline. The Stevens Lab at Boston Children’s Hospital has provided vital insights into how these immune cells behave irregularly in Alzheimer’s patients, paving the way for potential therapeutic interventions that could restore their normal function and, as a result, aid in Alzheimer’s treatment.
Furthermore, understanding the dynamics of microglial cells is crucial for shaping new strategies to combat Alzheimer’s. As research led by Beth Stevens highlights, the delicate balance of microglial pruning needs to be maintained to ensure healthy neural networks. Their findings suggest that targeting the dysfunction of these cells could not only halt the progression of Alzheimer’s disease but might also be applicable to other neurodegenerative disorders. Such breakthroughs would not only advance Alzheimer’s research but also improve our strategies for early diagnosis through new biomarkers, ultimately benefitting millions facing the challenges of these diseases.
Innovative Therapies Arising from Neuroinflammatory Research
The groundbreaking research spearheaded by Beth Stevens at Boston Children’s Hospital is laying the groundwork for innovative treatments in the fight against Alzheimer’s disease. By elucidating the role of microglial cells in neuroinflammation, Stevens and her team have set the stage for potential pharmacological interventions designed to modulate these immune responses effectively. This line of inquiry could lead to medications that not only alleviate symptoms but also address the underlying pathophysiology of Alzheimer’s, significantly transforming patient care. As we continue to explore the complexities of neuroinflammation, the possibility of developing targeted therapies becomes increasingly viable.
In addition to potential drug therapies, the research emphasizes the need for comprehensive strategies that incorporate various treatment modalities. For example, lifestyle modifications that may enhance cognitive resilience can serve as a complementary approach alongside pharmacotherapy. Additionally, education initiatives aimed at improving public understanding of Alzheimer’s disease and its risk factors can foster early detection and management. The convergence of pioneering research and community awareness offers a hopeful horizon in the ongoing battle against Alzheimer’s, with Beth Stevens’ work serving as a beacon of progress.
The Future of Alzheimer’s Research: Collaborative Approaches
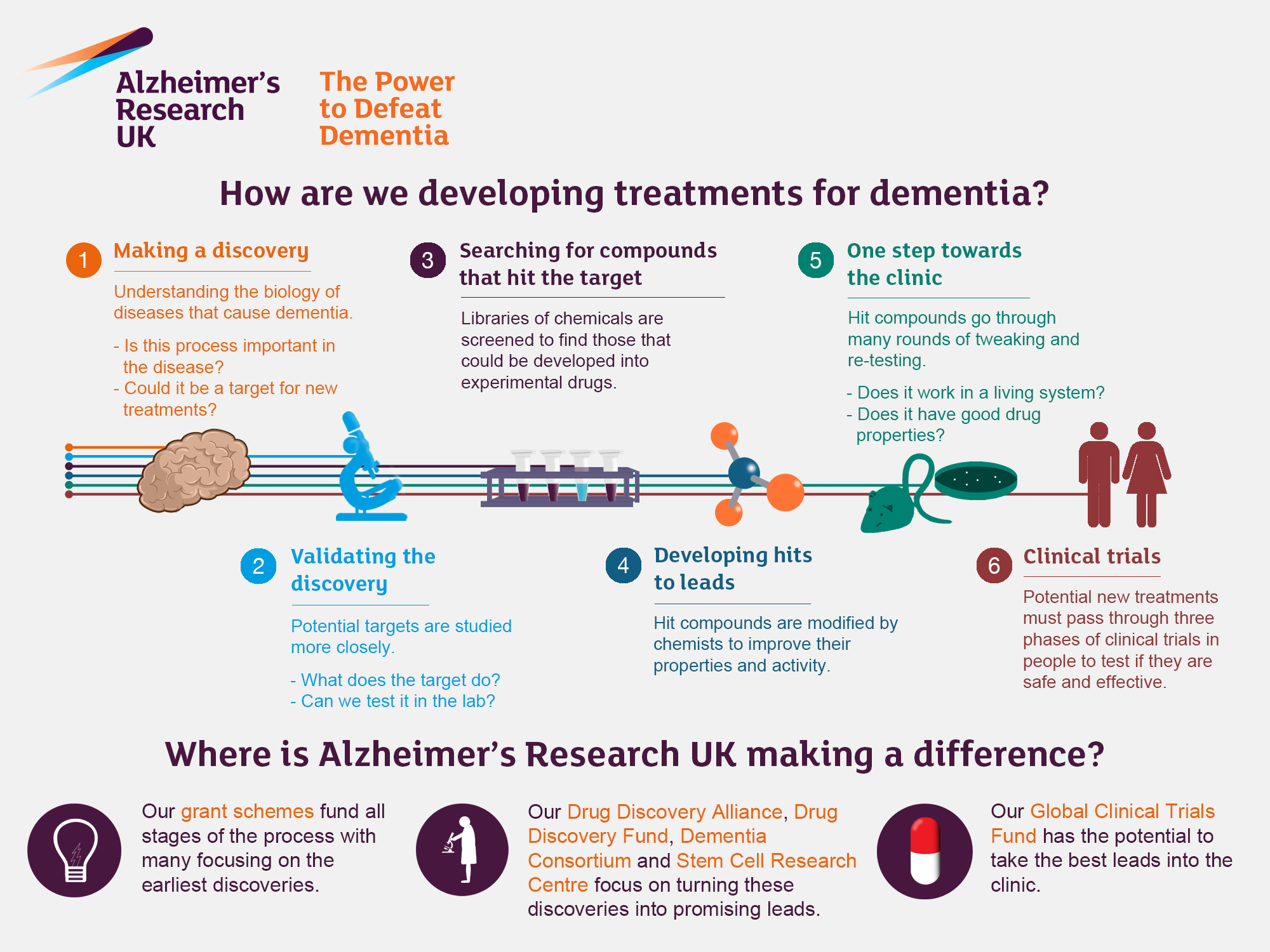
The future of Alzheimer’s research looks promising, buoyed by collaborative efforts among institutions, scientists, and funding agencies. The Stevens Lab has demonstrated that foundational research is often driven by interdisciplinary cooperation among neuroscientists, geneticists, and clinicians. This synergy is critical for developing a comprehensive understanding of Alzheimer’s disease and for exploring groundbreaking treatment options. Initiatives at Boston Children’s Hospital exemplify the power of collaborative science, bridging gaps between basic research and clinical applications, much needed to confront the complexity of neurodegenerative diseases.
Such collaborations extend to partnerships with organizations like the Alzheimer’s Association, which amplify the visibility and urgency of Alzheimer’s research. These collaborative networks enable the exchange of knowledge, resources, and expertise that can accelerate discoveries and enhance funding opportunities. With the imminent doubling of Alzheimer’s cases projected by 2050, fostering such partnerships is not just advantageous but essential. The path forward necessitates the unification of varied scientific perspectives to effectively address the global Alzheimer’s crisis, ultimately leading to impactful solutions for those affected.
Milestones in Alzheimer’s Treatment: Learning from History
Tracing the history of Alzheimer’s treatment reveals a long journey characterized by incremental discoveries. Researchers like Beth Stevens have built upon decades of foundational studies to unravel the mysteries surrounding Alzheimer’s disease. By learning from past approaches, the current research landscape is better equipped to explore innovative therapeutic options. From initial observations of amyloid plaques to the recent focus on the immune functions of microglial cells, each milestone has contributed invaluable knowledge towards developing multifaceted treatments. Such historical insights emphasize the importance of curiosity-driven science and its ability to bridge gaps in understanding and lead to transformative treatment strategies.
Moreover, the pursuit of knowledge in Alzheimer’s treatment reflects a gradual shift towards personalized medicine. By integrating genetic, lifestyle, and environmental factors, researchers aim to tailor interventions to the unique needs of individuals. As studies continue to explore the intricate relationships between microglial behavior and neural health, we can anticipate advancements that are increasingly bespoke. Looking ahead, integrating lessons from history with contemporary scientific techniques presents a promising path towards breakthroughs in Alzheimer’s treatment that can lead to significant improvements in patient outcomes.
The Economic Impact of Alzheimer’s Disease
Alzheimer’s disease not only poses profound personal and emotional challenges but also places a significant economic burden on families and healthcare systems. With the staggering projection of annual cases expected to double by 2050, the fiscal impact could escalate from $360 billion to over $1 trillion. The increasing prevalence of Alzheimer’s, driven by an aging population, calls for urgent action in Alzheimer’s research and innovation. As funding levels for basic science and technology development rise, the focus must remain on harnessing discoveries from labs like those at Boston Children’s Hospital to address these looming economic challenges.
In light of these economic implications, investments in Alzheimer’s research emerge as not just a health priority but also an economic imperative. By fostering advancements in biomarkers, diagnostics, and effective treatments, we can potentially reduce the long-term costs associated with care and improve the quality of life for millions. Understanding that the fight against Alzheimer’s disease has vast economic significance reinforces the urgency for innovative therapies that stem from current research. Ensuring science is adequately funded and prioritized will help mitigate the impending financial crisis associated with neurodegenerative diseases.
Beth Stevens: Pioneering New Paths in Neuroscience
Beth Stevens emerges as a leading figure in the neuroscience community, notably for her transformative work on microglial cells and their implications for neurodegenerative diseases. Her innovative research at Boston Children’s Hospital not only facilitates a deeper understanding of the immune mechanisms at play in Alzheimer’s disease but also bridges the gap between scientific inquiry and real-world application. Being recognized as a MacArthur genius underscores the significance of her contributions, illustrating how her work has propelled insights that could revolutionize Alzheimer’s treatment approaches.
As Stevens continues to challenge traditional perceptions of neuroinflammation and its role in Alzheimer’s, her dedication to scientific rigor inspires future generations of researchers. Her belief in following the science serves as a reminder of the importance of curiosity-driven research in uncovering novel treatments. With a fervent commitment to unlocking the complexities of the brain’s immune response, Stevens not only highlights the brilliance of basic science but also the profound impact it can have on improving health outcomes for individuals grappling with Alzheimer’s disease.
The Role of Federal Funding in Alzheimer’s Research
Federal funding has proven to be a cornerstone of advancements in Alzheimer’s research, empowering scientists like Beth Stevens to pursue innovative studies that can lead to transformative therapies. The support from organizations like the National Institutes of Health has provided the resources necessary for her lab to explore vital questions about microglial cells and their functions in neurodegenerative diseases. Such funding underscores the importance of public investment in science, without which many promising lines of inquiry would remain unexplored.
Moreover, sustained federal investment lays the foundation for long-term studies that can establish causative links between neuroinflammation and conditions like Alzheimer’s disease. As researchers continue to make strides, the necessity for ongoing financial support becomes increasingly clear, ensuring that important scientific questions can be addressed and that discoveries can be translated into effective treatments. The relationship between federal funding and breakthroughs in Alzheimer’s treatment accentuates the critical role that government initiatives play in shaping the future of neuroscience.
Early Detection: The Key to Alzheimer’s Combat
Early detection of Alzheimer’s disease is crucial for effective treatment and management. Research spearheaded by Beth Stevens at Boston Children’s Hospital has shed light on the potential biomarkers associated with neuroinflammation and microglial cell behavior, which could enable earlier diagnosis of this devastating condition. Utilizing advanced neuroimaging technologies and identifying biomarkers can facilitate timely interventions that significantly improve quality of life for patients and their families.
Furthermore, recognizing the initial stages of Alzheimer’s allows for a more proactive approach to treatment. By combining lifestyle changes, pharmacological interventions, and supportive therapies, stakeholders can create comprehensive care plans that address not only the symptoms but also the underlying processes contributing to the disease. With continued research efforts focused on enhancing early detection mechanisms, the path to managing Alzheimer’s could lead to improved outcomes and prolonged independence for those living with the disease.
The Intersection of Genetics and Alzheimer’s Research
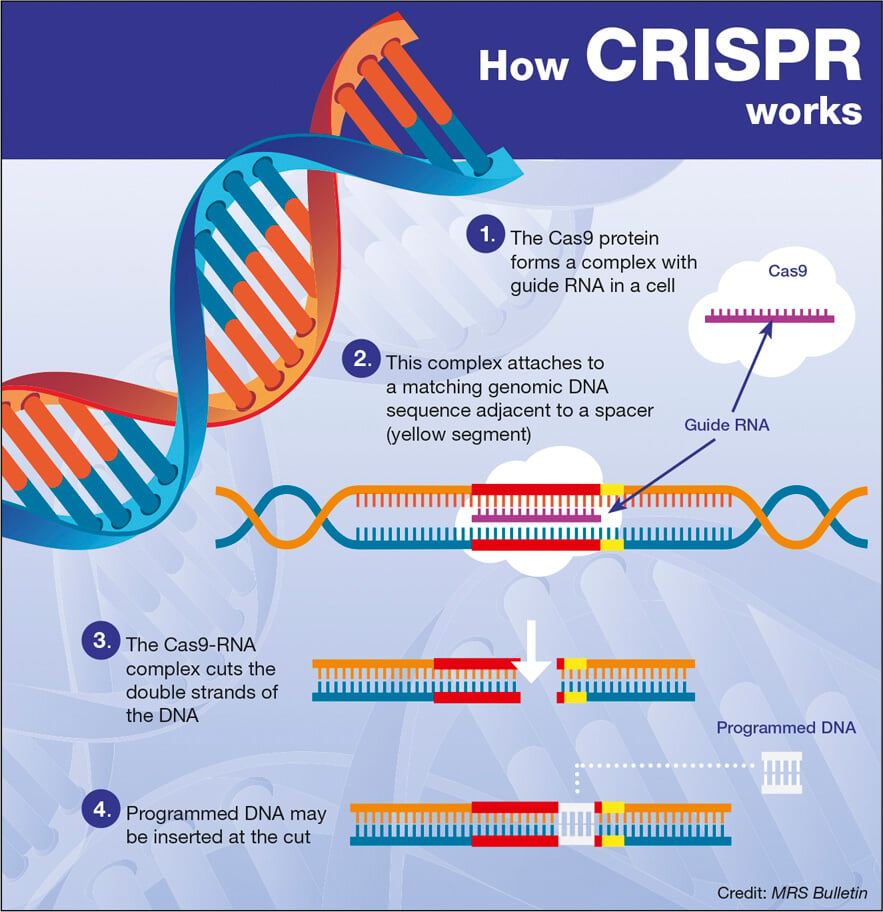
Genetics plays a pivotal role in understanding Alzheimer’s disease, as research indicates a significant hereditary component to the condition. By studying the genetics of Alzheimer’s patients, researchers like Beth Stevens have begun to unravel the complex biological pathways that predispose individuals to neurodegeneration. Understanding these pathways is essential in developing targeted therapies that consider genetic susceptibility, thereby personalizing treatment strategies that cater to individual patient profiles.
Moreover, integrating genetic data with studies on microglial cell behavior opens the door to novel interventions. As research continues to elucidate the genetic factors influencing microglial function and neuroinflammation, we can anticipate the emergence of precision medicine approaches that not only prevent but also interrupt the progression of Alzheimer’s disease. This intersection of genetics and neurobiology represents a promising frontier in Alzheimer’s research, ultimately aimed at transforming patient care and outcomes.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s research?
Microglial cells are crucial for Alzheimer’s research as they act as the brain’s immune system, identifying and eliminating damaged neurons. Recent studies, particularly from Beth Stevens at Boston Children’s Hospital, indicate that improper pruning by these cells may contribute to neurodegenerative diseases, including Alzheimer’s. Understanding these processes is vital for developing targeted Alzheimer’s treatments.
How can Beth Stevens’ research contribute to Alzheimer’s treatment?
Beth Stevens’ research at Boston Children’s Hospital highlights how microglial cells influence synapse pruning, which is linked to Alzheimer’s disease. By exploring these mechanisms, her lab aims to identify new biomarkers for early detection and therapies that could mitigate the effects of Alzheimer’s and other neurodegenerative diseases.
What advancements have been made in Alzheimer’s research related to microglial function?
Recent advancements in Alzheimer’s research, particularly in the work of Beth Stevens, reveal that microglial function is pivotal in the progression of Alzheimer’s disease. Her studies indicate that aberrant synaptic pruning by microglia may lead to neuronal loss, underscoring the need to focus on these cells for potential Alzheimer’s treatments.
What is the significance of Boston Children’s Hospital in Alzheimer’s research?
Boston Children’s Hospital is significant in Alzheimer’s research as it is home to leading scientists like Beth Stevens, who explore the role of microglial cells in brain health and disease. The insights gained from this research are critical for developing therapeutic strategies for Alzheimer’s and similar neurodegenerative conditions.
Why is research on neurodegenerative diseases like Alzheimer’s crucial?
Research on neurodegenerative diseases like Alzheimer’s is vital to address the growing public health challenge posed by an aging population. With millions affected and projections indicating a doubling of cases by 2050, understanding the mechanisms of diseases like Alzheimer’s can lead to preventive measures and effective treatments.
How does aberrant pruning by microglial cells impact Alzheimer’s development?
Aberrant pruning by microglial cells can lead to synaptic dysfunction and neuronal death, crucial factors in Alzheimer’s development. By studying these processes, researchers aim to uncover pathways that can be targeted for new Alzheimer’s treatments, potentially improving outcomes for those affected.
What funding does Alzheimer’s research require, as seen in Beth Stevens’ work?
Alzheimer’s research, such as that conducted by Beth Stevens, often relies heavily on federal funding from institutions like the National Institutes of Health. This support is essential for exploring complex scientific questions related to Alzheimer’s and discovering innovative therapeutic strategies.
What future directions are suggested by current Alzheimer’s research?
Current Alzheimer’s research suggests future directions may include targeted therapies aimed at modulating microglial function and refining early diagnostic biomarkers. The ongoing studies led by innovators like Beth Stevens at Boston Children’s Hospital could pave the way for breakthroughs in understanding and treating Alzheimer’s.
| Key Point | Details |
|---|---|
| Microglial Cells | These act as the brain’s immune system, clearing out debris and pruning synapses. |
| Aberrant Pruning | Faulty pruning can exacerbate conditions like Alzheimer’s and Huntington’s diseases. |
| Impact on Treatment | Research has led to new medicines and biomarkers to detect neurodegenerative diseases earlier. |
| Research Funding | Significant funding from NIH and federal agencies has supported pivotal findings in this field. |
| Aging Population | With 7 million Americans living with Alzheimer’s, cases are expected to double by 2050. |
| Basic Science Importance | Exploratory research, even if not directly disease-related, cultivates innovative treatments. |
Summary
Alzheimer’s research is at a pivotal point, with groundbreaking discoveries enhancing our understanding of the disease. Dr. Beth Stevens’ work on microglial cells highlights the critical role these immune cells play in brain health, especially in relation to neurodegenerative diseases like Alzheimer’s. Her findings not only contribute to the development of potential new treatments but also stress the importance of basic scientific research in uncovering complex health issues. As the population ages and the prevalence of Alzheimer’s increases, such research remains vital in our fight against this challenging disease.