Pediatric cancer recurrence poses a significant challenge in the treatment of young patients, particularly those diagnosed with brain tumors like gliomas. Recent advancements in artificial intelligence (AI) are changing the landscape, as studies reveal that AI tools can predict relapse risks with greater accuracy than conventional methods. Researchers at Mass General Brigham have developed an innovative AI model that utilizes temporal learning to analyze multiple brain scans over time, offering hope for more effective pediatric glioma treatment. Many of these tumors are treatable, yet the risk of cancer relapse remains a critical concern for families battling this disease. Improved predictive capabilities not only promise to enhance patient care but also alleviate the burdensome follow-up process that has traditionally involved frequent MRI scans for these vulnerable patients.
Childhood cancer relapse, especially in the context of brain tumors such as pediatric gliomas, represents a daunting hurdle for both patients and healthcare providers. Enhanced technologies in medical imaging, particularly through the use of AI, are ushering in new strategies for anticipating recurrence. By leveraging advanced algorithms that employ temporal learning techniques, researchers are uncovering more precise methods to monitor changes in patient conditions over time. This approach not only refines predictions related to cancer recurrence but also seeks to improve overall treatment protocols for children at risk. As science continues to evolve, the hope is that these innovative solutions will lead to better outcomes and forge new paths in pediatric oncology.
The Promise of AI in Pediatric Cancer Prediction
Artificial Intelligence (AI) is transforming the landscape of pediatric oncology, especially in predicting cancer relapse. Recent studies have shown AI’s capabilities to analyze complex data from numerous brain scans, which significantly enhances the ability to predict pediatric cancer recurrence. This evolution in technology facilitates more precise risk assessments compared to traditional methods. The integration of AI-driven tools in clinical settings could ultimately lead to tailored treatment strategies that benefit young patients battling illnesses like gliomas.
Moreover, AI applications extend beyond mere predictions; they can influence treatment pathways and patient care approaches. By continuously learning from vast datasets, AI can identify patterns that might be overlooked by clinicians, ensuring that children receive the most effective interventions when they are most beneficial. The future may hold substantial improvements in pediatric glioma outcomes as these advancements in AI are harnessed for proactive monitoring and personalized treatment, reducing the risks of devastating relapses.
Temporal Learning: A Game Changer in Medical Imaging
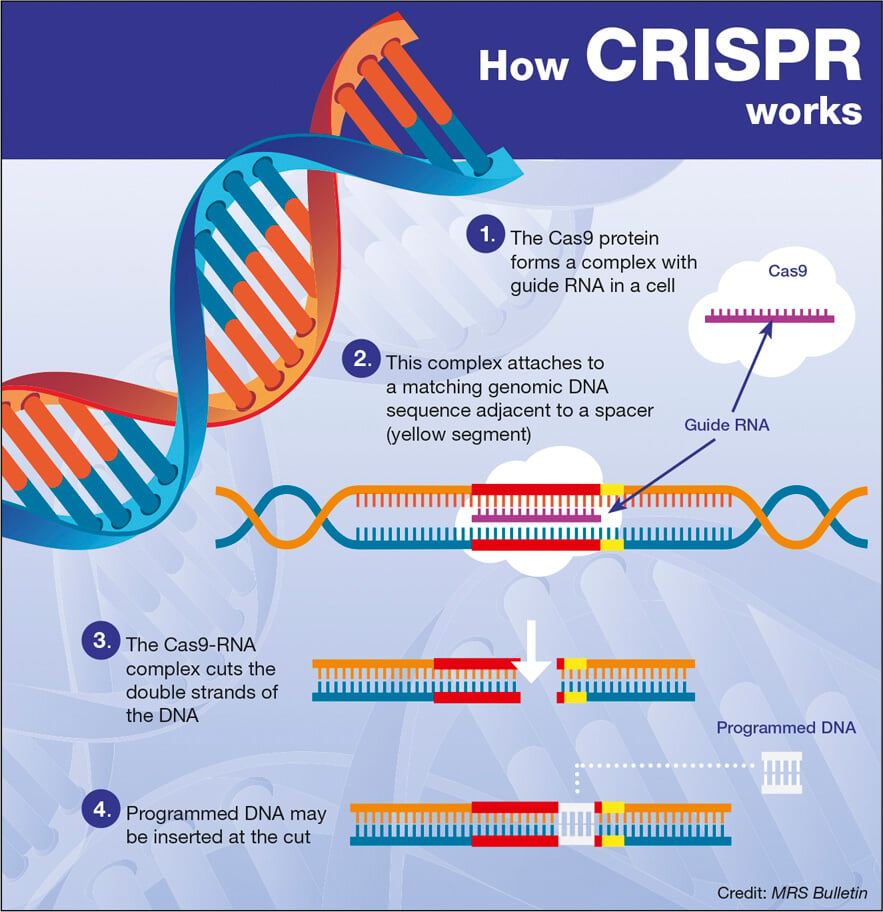
Temporal learning has emerged as a groundbreaking technique in the realm of medical imaging, particularly for children recovering from brain cancer. Unlike traditional models that analyze isolated scans, temporal learning synthesizes information from multiple scans over an extended timeframe. This innovative method drastically enhances prediction accuracy for cancer relapse by allowing AI to recognize subtle changes in tumor characteristics over time, significantly impacting decisions concerning patient monitoring and treatment.
In pediatric glioma cases, this two-pronged approach not only increases the precision of predictions related to pediatric cancer recurrence but also reduces stress on young patients and their families. By distinguishing between varying degrees of risk associated with low and high-grade gliomas, healthcare providers can tailor follow-up schedules and implement timely interventions. This promises a future where AI-enabled predictive insights lead to less invasive monitoring processes, ultimately improving the quality of life for pediatric cancer patients.
Understanding Glioma and Its Treatment Challenges
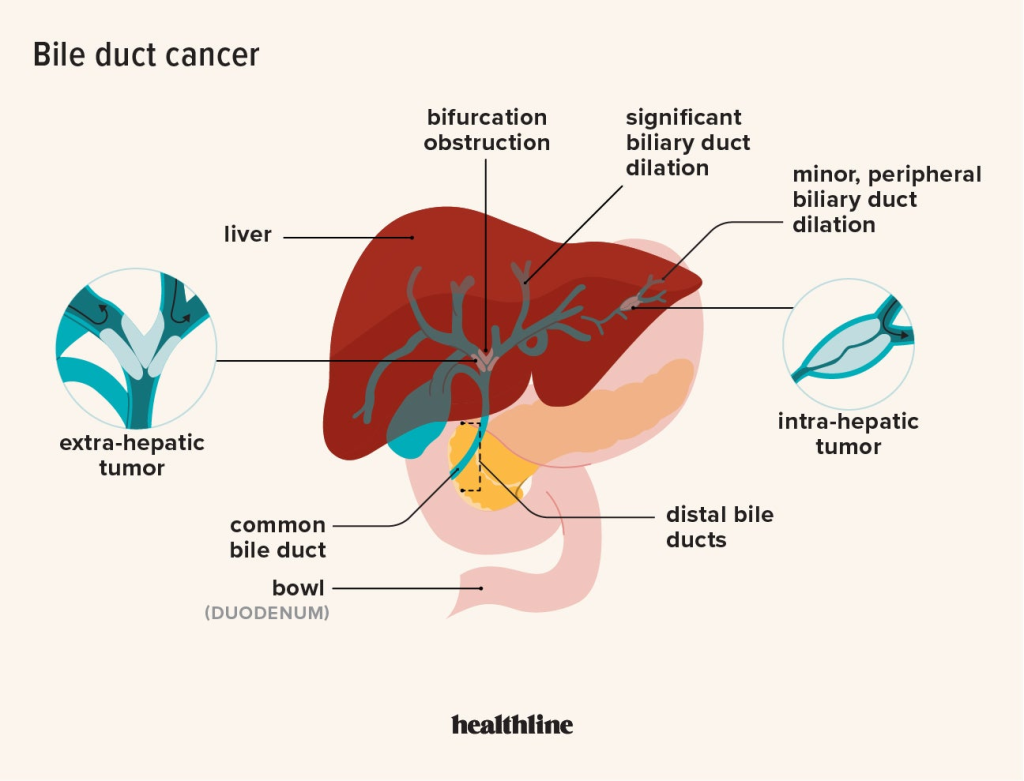
Gliomas are a type of tumor that arise from glial cells in the brain and are known for their unpredictability in terms of treatment success and recurrence. While many pediatric gliomas can be effectively treated with surgical intervention, the risk of recurrence is a pressing concern. The behavior of these tumors can vary significantly among individuals, necessitating the need for advanced predictive tools to assess the likelihood of osteosarcoma recurrence and strategy for follow-up care.
Treatment planning for gliomas includes a multidisciplinary approach, where oncologists, neurosurgeons, and radiation therapists collaborate to determine the best course of action post-surgery. However, the challenge lies in ensuring that these interventions are proactive rather than reactive. By utilizing AI technologies, healthcare teams can better stratify risk profiles for pediatric patients, enhancing their ability to deliver personalized therapy that addresses specific challenges associated with glioma recurrence.
AI-Driven Innovations in Pediatric Cancer Care
The integration of AI tools in pediatric cancer management represents a significant innovation, shifting the paradigm from conventional predictive models to sophisticated analytics that are capable of assessing real-time changes in patient conditions. As demonstrated in recent studies, AI models that utilize multiple imaging time points offer a more nuanced understanding of glioma progression, far outpacing traditional methods. This leap in technology not only increases detection rates for potential relapses but also streamlines the overall treatment process, affording clinicians the ability to intervene before critical complications arise.
AI’s role extends beyond prediction; it is becoming a cornerstone in the development of new therapies tailored to the specific needs of pediatric patients. By harnessing large datasets and identifying trends in treatment responses, AI can inform clinical trials that explore novel therapeutic strategies aimed at reducing the incidence of cancer relapse. As these innovations advance, we may witness significant shifts in how pediatric cancer, particularly gliomas, is managed in clinical practice.
The Role of Clinical Trials in Advancing AI Use
Clinical trials are integral to translating AI-driven cancer prediction models into everyday practice, particularly in the field of pediatric oncology. These trials facilitate the testing of AI tools in diverse patient populations, assessing their efficacy and safety in real-world contexts. The ongoing research, especially around tools developed for gliomas, aims not only to validate the AI predictions but also to refine the methodologies that are being employed. The findings from such trials could pave the way for broader adoption of AI technologies in standard care protocols.
Furthermore, successful implementation in clinical trials could lead to significant changes in how pediatric cancer treatment regimens are structured. By demonstrating that AI can reliably predict pediatric cancer recurrence and guide treatment decisions, researchers hope to reduce unnecessary imaging and allow for more focused therapeutic interventions. This represents a pivotal advancement in oncology that could reshape outcomes for young patients facing the challenges of glioma and other forms of pediatric cancer.
Reducing Stress Through Improved Predictive Models
One of the most significant benefits of developing AI tools for predicting pediatric cancer recurrence is the potential to alleviate the psychological and emotional burdens associated with treatment follow-ups. Regular imaging, a standard practice to monitor for potential relapses, often causes anxiety for both children and their families. By employing AI models that can provide accurate relapse predictions, healthcare providers can tailor follow-up schedules more appropriately, reducing the frequency of scans for those deemed at lower risk.
This innovative approach not only enhances the quality of life for families navigating the complexities of treatment but also fosters trust in the systems that are monitoring their child’s health. As families receive more precise information about their child’s prognosis, they can engage in more informed discussions about treatment options and follow-up care, ultimately leading to a more supportive and less stressful environment during a challenging period in their lives.
Ethical Considerations in AI-Enhanced Oncology
While the advancements in AI present remarkable opportunities in pediatric oncology, they also raise significant ethical questions that necessitate careful consideration. The deployment of AI-driven tools for predicting pediatric cancer recurrence must be accompanied by a robust framework addressing data privacy, informed consent, and potential biases in algorithmic predictions. Ensuring that AI systems treat all patients equitably, without inadvertently favoring certain demographics, is paramount in establishing trust among patients and providers alike.
Moreover, transparency in how AI models generate predictions is essential for fostering acceptance of these technologies among healthcare professionals and families. Open communication about the capabilities and limitations of AI tools ensures that patients are adequately informed when decisions about their treatment paths are made, thereby promoting shared decision-making. As the field of AI in medicine continues to evolve, the focus must equally address these ethical challenges alongside technological advancements.
Future Directions in Pediatric Cancer Research
The field of pediatric oncology is on the brink of transformation, with significant emphasis being placed on harnessing AI for improved patient outcomes. Future research must continue to explore the potential of AI technologies, not only in predicting pediatric cancer recurrence but also in refining treatment methodologies across various cancer types. Innovations such as machine learning models and advanced imaging analysis techniques hold the promise of revolutionizing how healthcare providers approach pediatric cancer care.
Furthermore, interdisciplinary collaborations among hospitals, research institutions, and technology firms will be crucial as we move towards a more integrated approach in treating childhood cancers like gliomas. By pooling resources and knowledge, the medical community can accelerate advancements that result in not just better predictive tools, but also comprehensive treatment frameworks that are sensitive to the unique needs of pediatric patients. The future of pediatric oncology shines brightly with the potential for AI to make a profound impact on diagnosis, treatment, and long-term outcomes.
Educating and Empowering Families in Pediatric Oncology
As the landscape of pediatric oncology continues to evolve, educating families about the role of AI in managing pediatric cancer recurrence is essential. Empowerment through knowledge can help parents feel more confident in navigating their child’s treatment journey. Providing clear information on how AI tools operate and how they will influence their child’s care can alleviate fears and uncertainty about new technologies. It is vital that families are kept in the loop and understand the importance of early intervention and ongoing monitoring.
Additionally, fostering a partnership between healthcare providers and families is crucial for ensuring that patients receive comprehensive care. Encouraging open dialogues and educational sessions about AI can enhance patient compliance and trust in treatment plans, as families become active participants in their child’s health journey. This movement towards informed family engagement has the potential to optimize pediatric cancer care and improve overall outcomes for affected children.
Frequently Asked Questions
What is pediatric cancer recurrence and how does it relate to glioma prediction?
Pediatric cancer recurrence refers to the return of cancer in children after treatment. In the context of glioma prediction, new AI tools enhance the ability to predict the relapse risk of childhood brain tumors known as gliomas, improving patient care by identifying those at high risk of recurrence earlier.
How does AI improve the prediction of pediatric cancer recurrence compared to traditional methods?
AI improves the prediction of pediatric cancer recurrence by analyzing multiple brain scans over time using temporal learning techniques. This allows for a more nuanced understanding of changes in the patient’s condition, resulting in significantly higher accuracy in predicting cancer relapse than traditional single-image methods.
What role does temporal learning play in pediatric glioma treatment and recurrence prediction?
Temporal learning is crucial in pediatric glioma treatment as it enables AI models to utilize multiple sequential brain scans taken post-surgery. By understanding how the tumor environment changes over time, the model can more accurately predict pediatric cancer recurrence, aiding in more effective management of glioma patients.
What are the implications of improved cancer relapse AI predictions for pediatric patients?
The implications of improved cancer relapse AI predictions are profound; they can lead to tailored follow-up care, reducing unnecessary imaging for low-risk patients while enabling more aggressive monitoring and treatment for those identified as high-risk for pediatric cancer recurrence.
Are the AI tools developed for pediatric cancer recurrence predictions ready for clinical use?
While the AI tools developed for predicting pediatric cancer recurrence show promising results, further validation across various healthcare settings is necessary before they can be implemented clinically. Future trials will determine their effectiveness in real-world scenarios.
How does the accuracy of AI predictions for pediatric cancer recurrence compare to traditional imaging methods?
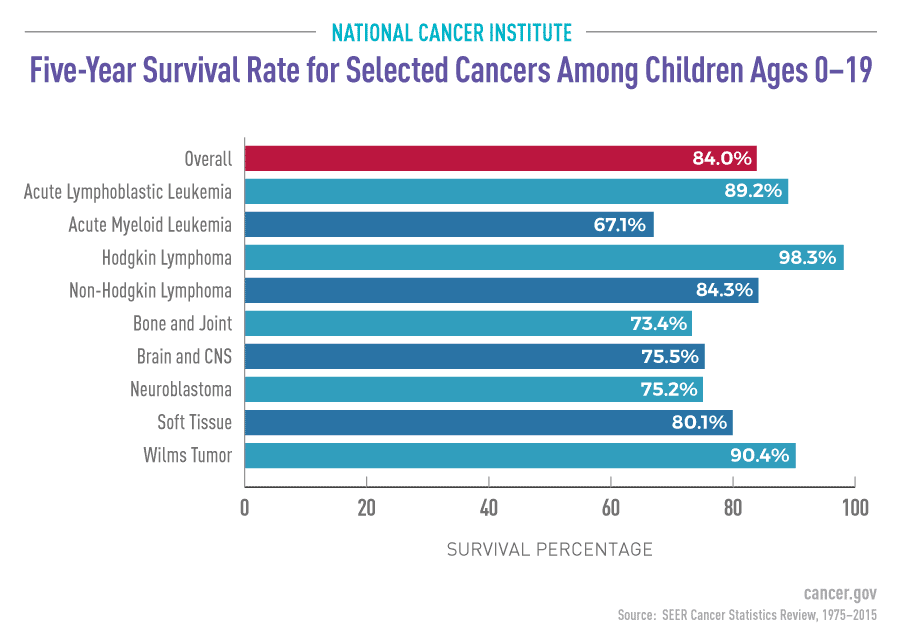
AI predictions for pediatric cancer recurrence reveal an accuracy of 75-89% using temporal learning techniques, which is a significant improvement over traditional imaging methods that yield only about 50% accuracy, indicating a substantial advancement in glioma management.
What future advancements can be expected in the field of AI in pediatric cancer?
Future advancements may include the widespread application of temporal learning models in various imaging contexts, leading to more personalized and effective treatment strategies for children with pediatric cancers, particularly in managing the risk of recurrence.
| Key Points | Details |
|---|---|
| AI Tool for Predicting Relapse | An AI tool that analyzes multiple brain scans has shown to predict relapse risk in pediatric cancer patients with greater accuracy compared to traditional methods. |
| Study Findings | The tool predicted recurrence of both low- and high-grade gliomas with an accuracy of 75-89%, significantly better than the 50% accuracy from single-image predictions. |
| Temporal Learning Technique | This innovative method trained the AI to analyze multiple scans taken over time, allowing it to recognize subtle changes and make more informed predictions. |
| Need for Improved Tools | Better prediction tools are necessary to reduce the burden of frequent follow-ups on families and to identify high-risk patients earlier. |
| Future Applications | Following further validation, the researchers aim to conduct clinical trials to enhance patient care for those at high risk of recurrence. |
Summary
Pediatric cancer recurrence is a critical issue in the management of young patients diagnosed with gliomas. Recent advancements in AI technology have greatly improved the ability to predict potential relapse, with researchers finding that multiple brain scans analyzed over time can enhance accuracy. This innovative approach promises to reduce the psychological and physical burdens on children and families by identifying high-risk patients more effectively. As this research progresses toward clinical trials, the potential for targeted therapies based on accurate AI predictions represents a significant advancement in pediatric oncology.